Sunday, May 31, 2009
The Medical History: Easy ways to approach and an uneasy task

Friday, April 3, 2009
A diet to control autism? Welcome to the GFCF diet
Sunday, February 8, 2009
Intellectual disability: New name for an old problem???
 It is never easy for any one to deal with a child with mental retardation. It is hard for the child no doubt, but equally hard for the parent to come to terms with the fact, and harder still for the dentist to approach the subject with the parent.
It is never easy for any one to deal with a child with mental retardation. It is hard for the child no doubt, but equally hard for the parent to come to terms with the fact, and harder still for the dentist to approach the subject with the parent. Intellectual disability: The Evolution of the term
Founded in 1876, AAIDD is the world's oldest and largest interdisciplinary organization of professionals concerned about mental retardation and related developmental disabilities. With headquarters in
AAIDD has updated the definition of mental retardation ten times since 1908, based on new information, changes in clinical practice, or breakthroughs in scientific research. The 10th edition of Mental Retardation: Definition, Classification, and Systems of Supports (2002) contains a comprehensive update to the landmark 1992 definition and provides important new information, tools, and strategies for the field and for anyone concerned about people with intellectual disability.
What is Intellectual disability?
Intellectual disability is a disability characterized by significant limitations both in intellectual functioning and in adaptive behavior as expressed in conceptual, social, and practical adaptive skills. This disability originates before the age of 18.
What causes intellectual disability?
Category | Type | Examples |
Prenatal | Chromosomal disorders | Downs syndrome*, Fragile X syndrome, |
| Single gene disorders | Inborn errors of metabolism, such asgalactosemia*, phenylketonuria*,mucopolysaccaridoses |
| Other conditions of genetic origin | Rubistein Tabi syndrome De Lange syndrome |
| Adverse material / environmental influences | Deficiencies* , such as iodine deficiency and folic acid deficiency |
Perinatal (around the time of birth) | Third trimester ( late pregnancy) | Complications of pregnancy* |
Labour (during delivery) | Severe prematurity, very low birth weight, birth | |
Neonatal (first four weeks of life) | Septicemia, severe jaundice*, hypoglycemia | |
Postnatal (in infancy and childhood) |
| Brain infections such as tuberculosis, Japanese |
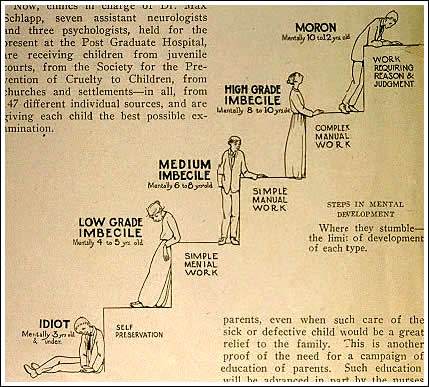
Intelligence Testing - IQ and the feasabilty of IQ testing
Galton's ideas on intelligence were influenced also by the work of a Belgian statistician named Lambert Adolphe Jacques Quetelet. Quetelet was the first to apply statistical methods to the study of human characteristics, and actually discovered the concept of normal distribution. However Galton's irrational belief in races with "superior" intellect led to the development of biased and often blatantly unfair tests.
It was a Frenchman named Alfred Binet who in 1904 developed the first objective

intelligence test. Commissioned by the French government to come up with a test to differentiate between children who had an inferior intellect and those who were normal.Binet's test simply put evaluated the average tasks that should be performed by a child of a given age to obtain mental age. This was then divided by the chronological age and multiplied by 100 to get the IQ. This simple formula to date remains the backbone of intelligence testing. Binet's work was brought to America and modified at Stanford University by Lewis M. Terman , and thus the famous "Stanford-Binet" intellegence test was born. The fourth edition of this test the SB-IV is still widely used.
Friday, January 30, 2009
Antibiotic Prohylaxis : Does it Work
- History
- Rationale
- Changes made and the reasons for those changes
- Clinical Implications
History of the anitbiotic prophylaxis regimen
 from Wilson W et.al Prevention of infective endocarditis: Guidelines from the American Heart Association: A guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group
from Wilson W et.al Prevention of infective endocarditis: Guidelines from the American Heart Association: A guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working GroupRationale of antibiotic prophylaxis in dentistry